From time to time we publish articles on topics that are of particular interest to our clients. Enjoy!
Featured Articles
- Article 1: Meeting the Challenge of Monitoring Medications in Older Adults by Anne Rich MSN, RN
- Article 2
- Article 3
- Article 4
Article 1: Meeting the Challenge of Monitoring Medications in Older Adults by Anne Rich MSN, RN
Takeaways:
- Monitoring medications in older adult patients can be challenging.
- Use an evidence-based approach to help your patients avoid adverse drug events.
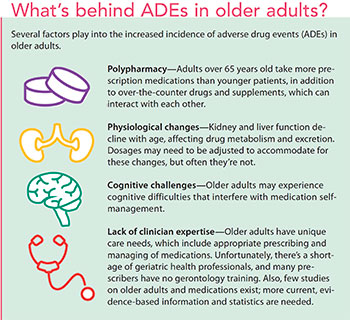 Many older adults have at least one chronic disease or condition and take multiple medications. In addition, they’re likely to see more than one prescribing physician and use more than one pharmacy, making tracking medications and identifying contraindications difficult. Older adults are more likely than younger adults to have a serious adverse drug event (ADE) that requires hospitalization. (See What’s behind ADEs in older adults?) Prescriptions of potentially inappropriate medications (PIMs) in the elderly also is a problem; for example, a 2016 study found that 29% of patients in a cardiology outpatient department were prescribed at least one PIM.
Many older adults have at least one chronic disease or condition and take multiple medications. In addition, they’re likely to see more than one prescribing physician and use more than one pharmacy, making tracking medications and identifying contraindications difficult. Older adults are more likely than younger adults to have a serious adverse drug event (ADE) that requires hospitalization. (See What’s behind ADEs in older adults?) Prescriptions of potentially inappropriate medications (PIMs) in the elderly also is a problem; for example, a 2016 study found that 29% of patients in a cardiology outpatient department were prescribed at least one PIM.
Despite the evidence, many older adults continue to be prescribed PIMs and end up suffering costly, and often preventable, ADEs. Studies in ambulatory and long-term care settings have found that 27% of ADEs in primary care and 42% in long-term care were preventable.
Older adults’ unique care needs require appropriate medication management. Nurses can help ensure patient safety by closely monitoring and regularly reviewing their patients’ medications. Perform a medication assessment at least every 6 months (more often if the patient has been acutely ill) and after every hospitalization. Document each review, the results, and planned actions in the patient’s health record. Two tools, the Beers Criteria for Potentially Inappropriate Medication Use in Older Adults (Beers Criteria) and the Brown Bag Review, can be used to aid in these assessments.
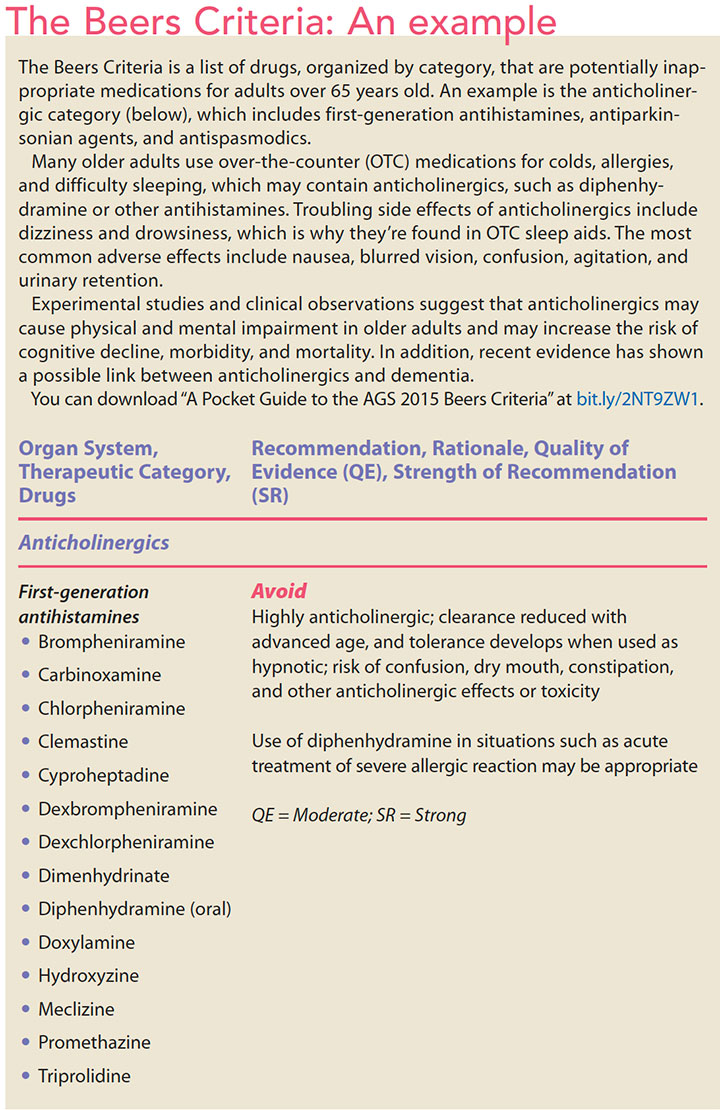
The Beers Criteria
In 1991, Dr. Mark Beers and his colleagues created a list of criteria for identifying medications whose risks outweigh their benefits and those that should be avoided or used with caution in adults 65 years and older. The American Geriatrics Society (AGS) revises and updates the criteria every 3 years, most recently in 2015. The AGS and an interprofessional panel of 13 geriatric care and pharmacotherapy experts comprehensively and systematically review and grade an extensive list of medications for drug-related problems and ADEs in older adults. Fifty-three medications or medication classes are included in the latest updated Beers Criteria, which contains these sections:
- PIMs and classes to avoid in older adults
- PIMs and classes to avoid in older adults with certain diseases and syndromes that the listed drugs can exacerbate
- medications to be used with caution in older adults
- potentially clinically important non-anti-infective drug-drug interactions that should be avoided in older adults.
Several organizations, including the Centers for Medicare & Medicaid Services, the National Committee for Quality Assurance, and the Pharmacy Quality Alliance, have identified the Beers Criteria as an important quality measure.
The criteria are intended as guidelines for prescribers and a clinical tool for nurses and other healthcare professionals to improve medication safety in older adults. (See The Beers Criteria: An example.) Use the criteria in combination with your clinical judgment and collaboration with patients and other members of the healthcare team to individualize care and treatment.
Brown Bag Review
The Brown Bag Review gives healthcare professionals an opportunity to review and discuss a patient’s medications. Ask your patient to bring in all medications they take, including every over-the-counter (OTC) product (pills, creams, ointments, vitamins, and supplements). Remind your patient to include medicines they may not take every day or may take only when they have symptoms. If you’re doing an assessment in the home, ask the patient for permission to check kitchen and bathroom cabinets and bedside tables and drawers for medicines he or she may have forgotten.
If any of the patient’s medications appear on the Beers Criteria list, bring them to the primary care provider’s (PCP) or prescriber’s attention. Frequently, patients don’t tell their PCP or other healthcare providers every medication they’re taking and forget they need to include all OTC medications and supplements. Another resource is the pharmacist. (If the patient isn’t hospitalized, you can contact the pharmacist at the location where the patient obtains his or her medications.)
During the Brown Bag Review, ask the patient to tell you why he or she is taking each medicine (thisterm is more readily understood than medication), when it’s taken, and how much is taken. If the patient is using a medication incorrectly, find out why and clarify what should be done. Use the teach-back method to verify the patient’s understanding.
Be a good detective
Pay attention, ask the right questions, insist on knowing every medication your older adult patients are taking, and use the Beers Criteria to closely monitor the appropriateness of those medications. These simple steps can help decrease the incidence of ADEs and promote better patient outcomes.
Anne Rich is a nurse educator and comprehensive care manager at Diversified Nurse Consultants, LLC in New Albany, Indiana.
Selected references
2012 Beers Criteria update: How should practicing nurses use the criteria? J Gerontol Nurs. 2012;38(6):3-5.
Agency for Healthcare Research and Quality. Health literacy universal precautions toolkit, 2nd ed. Conduct brown bag medicine reviews: Tool #8. February 2015.
Alternatives for Medications Listed in the AGS Beers Criteria for Potentially Inappropriate Medication Use in Older Adults. Health in Aging Foundation. 2015. healthinaging.org/files/documents/tipsheets/BeersAlternatives _2015.pdf
Olsson IN, Wätterbjörk I, Blomberg K. Registered nurses’ perception of their professional role regarding medication management in nursing care of the elderly. J Nurs Educ Pract. 2014;4(2):153-61.
Shah KN, Joshi HM, Christian RP, Patel KP, Malhotra SD. Prevalence of potentially inappropriate medications and prescription cost analysis among older cardiac patients in an outpatient department of a tertiary care hospital in India. J Basic Clin Pharm. 2016;7(4):110-5.
Xiong GL. Geriatric sleep disorder medication. Medscape. Updated December 21, 2017. emedicine.medscape.com/article/292498-medication
Published in American Nurse Today September 2018 Vol. 13 No. 9
Return to top
